Understanding Venous Stasis Disease: An In-Depth Guide
Venous stasis disease is a prevalent but often misunderstood condition that can significantly affect an individual's quality of life. This vascular issue arises due to improper functioning of vein valves, leading to blood pooling in the veins, particularly in the legs. Understanding the underlying mechanisms, symptoms, and treatments for this disease is crucial for effective management and prevention. In this comprehensive article, we will explore the various facets of venous stasis disease, empowering you with the knowledge to understand this condition better.
What is Venous Stasis Disease?
Venous stasis disease, often termed venous insufficiency, involves the condition where blood does not flow properly back to the heart from the limbs, primarily due to weakened valves in the veins. This often leads to a series of complications that can affect not only physical health but also emotional well-being.
Causes of Venous Stasis Disease
The causes of venous stasis disease can be multifactorial. Here are some of the primary contributors:
- Genetic Factors: A family history of vein problems can predispose individuals to develop venous stasis disease.
- Age: The risk increases with age due to the natural degradation of vein elasticity and valve function.
- Obesity: Excess body weight can lead to increased pressure on the veins, exacerbating the issue.
- Prolonged Sitting or Standing: Occupations that require long periods of inactivity can hinder blood flow and contribute to venous issues.
- Previous Blood Clots: History of deep vein thrombosis (DVT) can lead to damage in the vein structure, leading to venous stasis.
- Pregnancy: Hormonal changes and added pressure on the veins from the growing uterus can contribute to venous insufficiency.
Symptoms of Venous Stasis Disease
Recognizing the symptoms of venous stasis disease is essential for timely intervention. Common symptoms include:
- Swelling: Particularly in the legs and feet, which may worsen as the day progresses.
- Pain: Discomfort or aching in the legs, which may improve with elevation.
- Skin Changes: The skin may become discolored, dry, or itchy, leading to skin irritation.
- Varicose Veins: Enlarged veins that are visible under the skin’s surface.
- Ulcerations: Chronic sores can develop on the lower legs due to poor circulation.
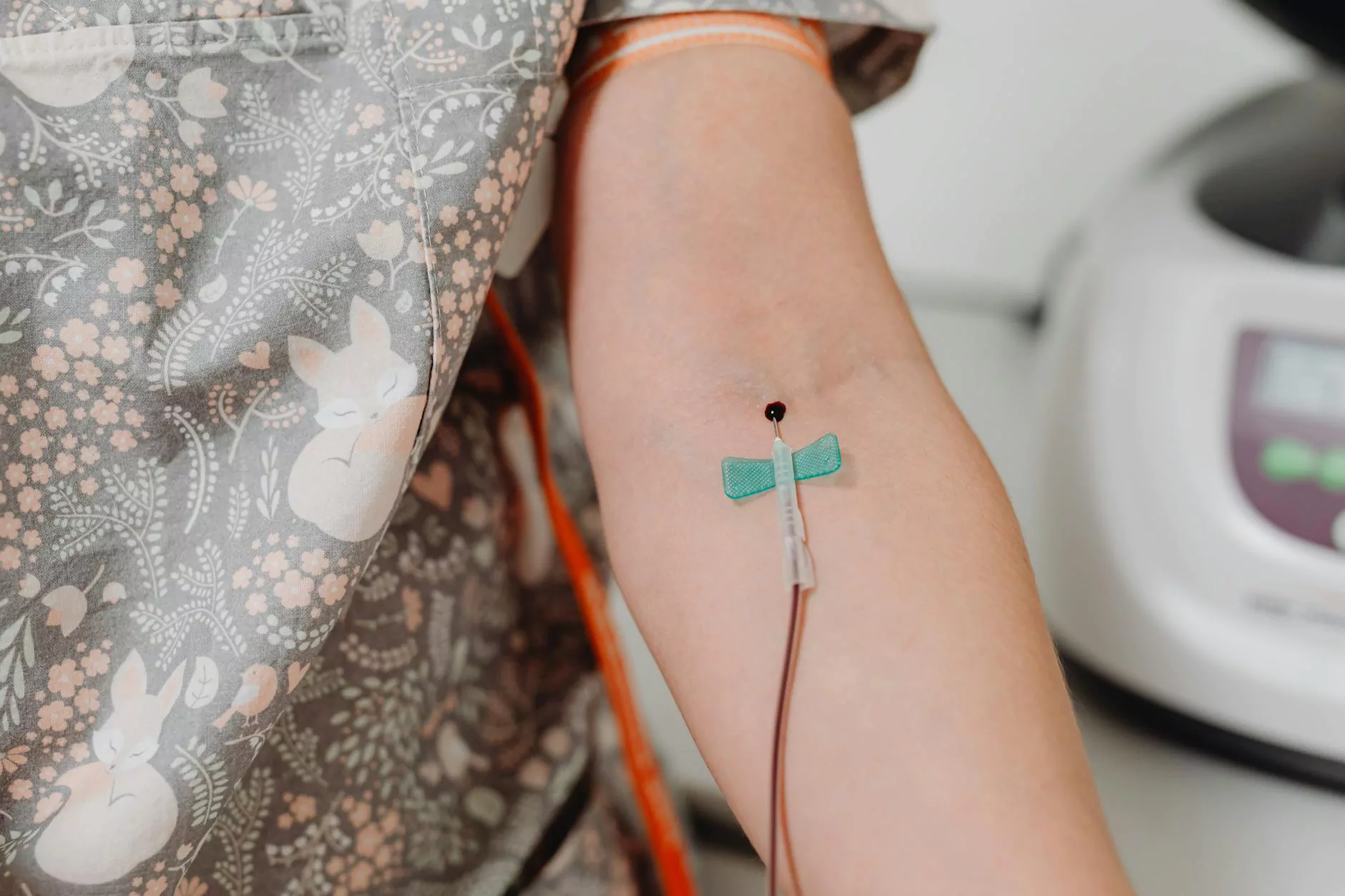
Diagnosing Venous Stasis Disease
Early diagnosis of venous stasis disease can significantly influence the treatment outcome. The diagnostic process typically involves:
- Physical Examination: A healthcare provider will assess symptoms and inspect the legs.
- Doppler Ultrasound: This non-invasive test measures blood flow in the veins and can identify any blockages or abnormalities.
- Venography: A specialized imaging test where a contrast dye is injected into the veins to visualize blood flow, although this is less commonly used today.
Treatment Options for Venous Stasis Disease
Treating venous stasis disease requires a multi-faceted approach, depending on the severity of the condition:
Non-surgical Treatments
- Compression Therapy: Wearing compression stockings can help improve circulation and reduce swelling.
- Medication: Anti-inflammatory medications may be prescribed to alleviate pain and swelling.
- Exercise: Regular physical activity is vital for enhancing blood flow and preventing further complications.
- Elevation: Elevating the legs can help reduce swelling and discomfort, especially after long periods of standing or sitting.
Surgical Treatments
In cases where non-surgical methods are ineffective, doctors may recommend surgical options, including:
- Endovenous Laser Treatment (EVLT): A minimally invasive procedure that uses laser energy to close off varicose veins.
- Vein Stripping: The surgical removal of the affected veins to improve blood flow.
- Ambulatory Phlebectomy: A procedure to remove varicose veins through small incisions in the skin.
Preventing Venous Stasis Disease
Preventing venous stasis disease is crucial, especially for individuals at risk. Here are practical tips to help reduce the chances of developing this condition:
- Maintain a Healthy Weight: This can alleviate pressure on the veins.
- Stay Active: Regular exercise promotes healthy circulation.
- Avoid Prolonged Standing or Sitting: If your job requires it, take regular breaks to walk or stretch your legs.
- Wear Compression Stockings: Especially if you spend long hours sitting or standing.
- Stay Hydrated: Proper hydration supports overall vascular health.
Living with Venous Stasis Disease
Living with venous stasis disease can be challenging, yet understanding the condition can empower affected individuals to manage their health effectively. Here are some lifestyle adjustments that may help:
- Regular Check-ups: Frequent visits to your healthcare provider can help monitor the condition and adjust treatment plans.
- Healthy Diet: Nutritional choices affect vascular health; a balanced diet rich in fiber can prevent obesity and other complications.
- Stress Management: Techniques such as yoga, meditation, and mindful activities can help reduce stress that may exacerbate symptoms.
Conclusion
Venous stasis disease represents a significant health concern, but effective management is within reach. By understanding the causes, symptoms, and treatment options available, you can take proactive steps to enhance your vascular health. Remember, if you experience symptoms indicative of this condition, seeking prompt medical attention is vital. By prioritizing your vascular wellness, you can lead a more active, fulfilling life. For more information on how to tackle venous stasis disease, we recommend visiting trufflesveinspecialists.com, where you can connect with experienced vascular specialists who can guide you further.